A magazine where the digital world meets the real world.
On the web
- Home
- Browse by date
- Browse by topic
- Enter the maze
- Follow our blog
- Follow us on Twitter
- Resources for teachers
- Subscribe
In print
What is cs4fn?
- About us
- Contact us
- Partners
- Privacy and cookies
- Copyright and contributions
- Links to other fun sites
- Complete our questionnaire, give us feedback
Search:
How do you solve a problem like arthritis?
by Jo Brodie, Hamit Soyel and Paul Curzon, Queen Mary University of London
Some diseases can't be cured. Doctors and nurses just try to control the disease to stop them ruining people's lives. Perhaps smartphone apps can pull off the trick of giving patients better care while giving clinicians more time to spend with the patients who most need them? A Venn diagram is at the centre of the Queen Mary team's prototype.
What is rheumatoid arthritis?
Normally your immune system does a good job of fighting infection and keeping you healthy. But, if you have an autoimmune disease, it can also attack your healthy cells, causing inflammation and damage. Rheumatoid arthritis is like this: a painful condition that mostly affects hands, knees and feet as the person's immune system attacks their joints, making them swell painfully. It affects around 400,000 people in the UK and is more common in women than men.
People with the disease alternate between periods when it is under control and they have few symptoms, and with days or weeks of painful 'flares' where it is very, very bad. During these flares it especially affects a person's ability to live a normal life. It can be hard to move around comfortably, do exercise - plus it interferes with their ability to work. It can also leave them totally reliant on family and friends just to do everyday things like dress or eat, never mind go out. This can lead to depression and puts a strain on friendships.
Treating the disease
Treatment, which can include tablets, injections, physiotherapy and sometimes surgery, slows the disease, keeping it under control for long periods. Sufferers are also given advice on lifestyle changes. This all reduces the risk of joint damage and helps people live their life more fully.
At appointments, doctors collect information to help them see how the disease is progressing. A Disease Activity Score (DAS) calculator lets them combine measurements for pain, how tender or swollen their patient's joints are and how many joints are affected. Regular blood tests keep track of the amount of inflammation and how the body is reacting to drugs. This helps them decide if they need to adjust the medication.
If it is caught early, modern medicine reduces the worst effects of the disease, helped by keeping a close eye on the Disease Activity Score as treatments may need to be repeatedly adjusted to control flares. This requires regular hospital visits which uses up scarce healthcare resources and is very time-consuming for patients. It is hampered because hospital appointments may only happen twice a year due to the number of patients. Everyone wants to give more personalised care, but hospitals just can't afford to provide it.
Supporting doctors
So, what do you do when there just aren't enough doctors to see everyone as regularly as needed to maintain their patients' wellbeing? One solution is to use remote monitoring with an app on a patient's smartphone, so involving patients more directly in their own care. They can use such apps to regularly record their own disease activity measurements, sharing the information with their doctor to save visiting the hospital.
A smart app
This is an improvement, but the measurements still require expert monitoring and can take more of the doctor's time. However, if smartphones can actually be made to be, well, smart, then they could help give advice between hospital visits and alert the hospital team, when needed, so they can step in. This might involve, for example, loading the app with background knowledge about rheumatoid arthritis, expert knowledge from lots of doctors, and creating an artificial intelligence to use this information effectively for each patient.
Hospital specialists and computer scientists at Queen Mary are developing such a prototype based on Bayesian networks as the artificial intelligence core. Bayesian networks are based on reasoning about the causes of things and how likely different things are to be the cause of something being observed. Building the prototype involves finding out if patients and clinicians find such tools useful and acceptable (some people might find clinic visits reassuring, while some may be keener to avoid taking the time off work, for example).
Smart and patient centred
This still focusses on a clinician's view of treatment using drugs though. With a smartphone app we can perhaps do better and take the person's life into account - but how? The first step is to understand patient goals. Patients would need to be willing to share lots of information about themselves so that the software can learn as much as possible about them. Eventually, this might be done using sensors that automatically detect information: how much pain they are in, how stiff their joints are, how much they move around, how long it takes them to get out of a chair, how much sleep they get, how often they meet others, if and when they take their medicine, and so on. Rather than just focussing on medical treatment it can then focus advice 'holistically' on the whole person.
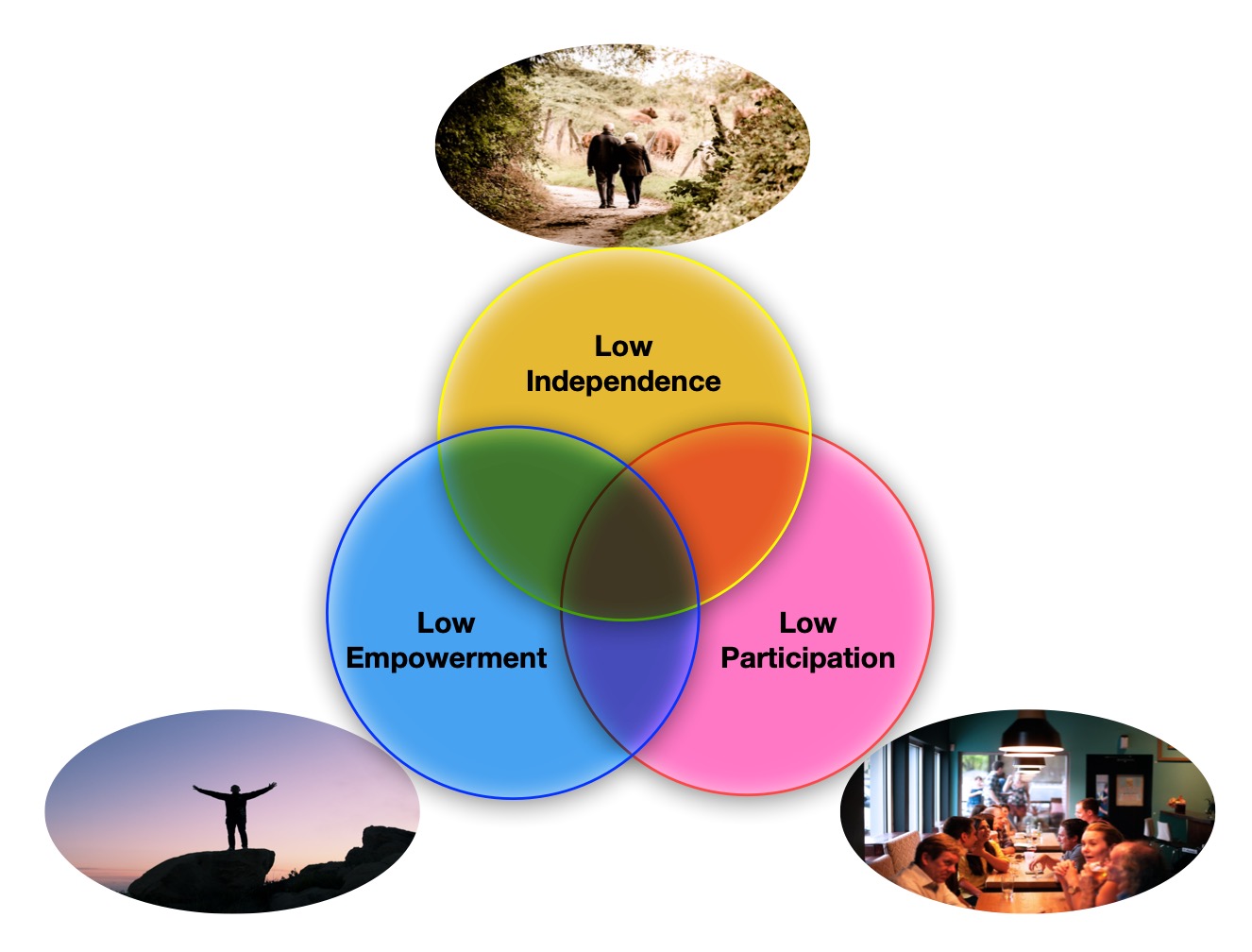
The Queen Mary team's approach is centred around three different things: helping people with physical independence so they can move around and look after themselves; empowering them to manage their condition and general well-being themselves; and participation in the sense of helping them socialise, keep friendships and maintain family bonds.
The Bayesian network processes the information about patients and computes their predicted levels of independence, empowerment and participation, working out how good or bad things are for them at the moment. This places them in one of seven positions in a Venn diagram of the three dimensions over which areas need most attention. It then gives appropriate advice, aiming to keep all three dimensions in balance, monitoring what happens, but also alerting the hospital when necessary.
So, for example, if the Bayesian network judges independence low, participation high and empowerment low, the patient is in the Venn diagram intersection of low empowerment and low independence. Advice in the following weeks, based on this area of the Venn diagram, would focus on things like coping with pain and stiffness, getting better sleep, as well as how to manage the disease in general.
By personalising advice and focusing on the whole person, it is hoped patients will get more appropriate care as soon as they need it, but doctors' time will also be freed up to focus on the patients who most need their help.


